Hormonal Therapy
Hormones are natural substances produced by the body that control reproduction, growth, and metabolism. A hormone is an internally secreted compound, such as insulin or thyroxine, formed in endocrine glands. Hormones affect the functions of specifically receptive organs or tissues when transported to them by the body fluids. Pharmaceutically, a hormone is a synthetic substance used in medicine to act like a compound when introduced into the body.
Hormones help regulate body mechanisms such as growth, metabolism, and reproduction.
Certain body tissues require hormones to develop. When cancer originates in these tissues it responds to hormone manipulation. By using substances that block the action of the hormones, it is possible to slow down, or even stop the growth of the cancer cells.
Hormones can be used to alter the growth of cancer. Cancer therapy, which achieves its anti-tumor effect through changes in hormonal balance, is also called endocrine therapy. Some tissues, such as prostate or breast, depend on hormones to develop. When a malignancy arises in these tissues, it is usually hormone responsive. Other primaries and histologic types may be hormone responsive, such as melanoma and hypernephroma. Hormonal therapy may affect the long-term control of the cancer growth.
Hormonal therapy is rarely given as a single agent with an intent to eradicate cancer. Hormones are often used to prevent or delay recurrence of cancer after other modalities of treatment such as surgery have removed the gross primary tumor and chemotherapy or radiation therapy have treated systemic and regional micrometastases.
An example is a breast cancer patient who had the primary tumor and positive axillary nodes removed surgically, received systemic chemotherapy and regional radiation, and was placed on tamoxifen, a synthetic antiestrogen, to prevent or delay recurrence.
Hormones can be administered orally, intravenously, or intramuscularly. Surgery may also be used to prevent the body from producing hormones. For example, a patient with prostate cancer may have an orchiectomy to prevent the production of testosterone.
Some types of cancer may originate from organs that require hormones to develop, but they may not be treated with hormonal therapy. A sample of the tumor can be sent to a special lab to determine if hormonal therapy is likely to be effective.
Since cancer is a genetic disease caused by DNA changes that control the functioning of cells, including how they grow and how they divide, it is important to discuss the relationship between genetics and cancer treatment. When there is alteration in the DNA either via inherited mutations or exposure to carcinogens, then cancer can develop and grow out of control. [2]
When cancer develops in an individual unique genetic change occur and genetics is the process by which these specific changes are identified. Understanding the genetics of a particular cancer helps target cancer treatment for that particular patient. For example, lung cancer patients with NSCLC who have an EGFR (epidermal growth factor receptor) mutation are likely to respond to drugs known as EGFR Inhibitors or a combination of therapies depending on specific mutations. [3]
Genetic testing is done to determine risk for certain types of hereditary cancer syndromes. Genetic testing is a type of laboratory test that looks for changes in chromosomes, genes, or proteins that may indicate an increased risk for cancer or other genetic disorder. The genetic test can confirm or rule out a suspected genetic condition such as BRCA1 or help determine a person's chance of developing or passing on a genetic disorder. The diagram below depicts a report that looks at genetic and cancer risk.
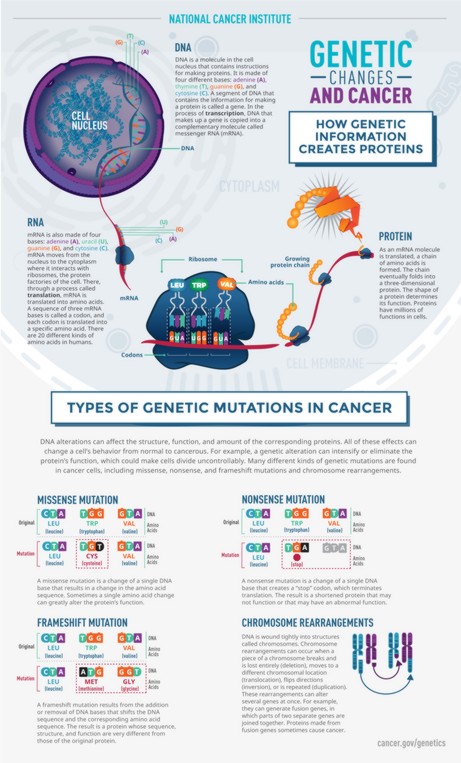
Genetic Changes and Cancer.
Source: National Cancer Institute (NCI).
Updated: December 21, 2023
Suggested Citation
SEER Training Modules: Hormonal Therapy. U.S. National Institutes of Health, National Cancer Institute. Cited 10 February 2026. Available from: https://training.seer.cancer.gov.




