Stem Cell Transplants
A bone marrow transplant (BMT) is the removal of bone marrow from one person and the return of its blood-forming cells later to the same person or the transfer of the blood-forming cells to someone else. It is a medical procedure used to treat diseases such as
- aplastic anemia
- Hodgkin's Lymphoma
- immune deficiency disorders
- leukemia
- multiple myeloma
- some solid tumors such as Ewing sarcoma and medulloblastoma
Bone marrow is the soft, sponge-like tissue found within the cavities of bones that contain fat and blood-forming tissue. It contains immature cells called stem cells that produce the body's blood cells. These blood cells include
- white blood cells (leukocytes), which fight infection
- red blood cells (erythrocytes), which carry oxygen to, and remove waste products from, organs and tissues
- platelets, which enable the blood to clot
Stem cells can also be collected from the peripheral blood in a process called "apheresis" and is much easier to collect than the stem cells from the bone marrow. Many patients receiving stem cell transplants today have the stem cells obtained from the peripheral blood, which is called "Peripheral Blood Stem Cell Transplant (PBSCT)." Stem cells can also come from umbilical cord blood.
Healthy bone marrow tissue constantly renews the blood supply and is essential to life. Unfortunately, the amount of drugs or radiation needed to kill cancer cells also destroys bone marrow. Bone marrow transplantation or stem cell transplant is often used as a rescue procedure, replacing stem cells that have been destroyed by high doses of chemotherapy and/or radiation therapy. In some cancers, particularly those involving the blood cells, bone marrow transplantation is used to attack the malignancy directly. Acute leukemia, for example, was the first cancer to be successfully treated with bone marrow transplantation.
The transplant procedure begins with the patient or donor providing stem cells. These blood-forming cells are stored while the patient's cancer cells are destroyed by chemotherapy drugs and/or radiation. The stem cells are then returned to the patient to speed the recovery of bone marrow.
Most bone marrow transplantation procedures are successful. The recipients are discharged promptly from the hospital after they have recovered. The long-term response rate varies greatly depending on the type and stage of cancer.
There are three types of transplants according to the source of the stem cells.
- Autologous - An autologous transplant is the removal of bone marrow from the person with cancer before treatment and is returned to him/her after treatment with high doses of chemotherapy or radiation therapy or both
- Allogeneic - An allogeneic transplant is donated by someone other than the patient or an identical twin. Siblings are always a closer match than parents and more likely to be compatible than other family members. The best matches also come from someone of the same ancestry
- Syngeneic - In syngeneic transplants, patients receive stem cells from their identical twin
As with some other cancer therapies, bone marrow transplants may also cause side effects, which should be recognized and effectively managed.
Almost everyone who undergoes bone marrow transplant experiences lethargy, nausea, and vomiting because of the high doses of chemotherapy and/or radiation that precede the transplant. Infection is an early serious danger for the patient, so the patient is closely monitored for fever and other signs of infection. Some patients may develop veno-occlusive disease, a very serious disease of the liver. Another major risk of bone marrow transplant is that the recipient's immune system may reject the transplanted "foreign" marrow.
Despite the risk involved with bone marrow transplant, the procedure is still recommended by physicians and opted for by cancer patients as an effective weapon against cancer. Most cancer patients receiving them benefit greatly from successful bone marrow transplants.
The specific type of stem cell procedure performed is documented in the registry abstract in the data item Hematologic Transplant and Endocrine Procedures. See the SEER Program Coding and Staging Manual 2018 for specific coding instruction and the CoC STORE manual.
Immune Cell Therapy - Immune cell therapy, which is also call "Adoptive Immunotherapy" or "Adoptive Cell Therapy" involves enhancing a patient's own immune cells ability to attack the cancer. This process involves removing the immune cells from the patient and growing large numbers of them in the lab then reinfusing them back to the patient. There are two approaches used for this process, which include
- Tumor-infiltrating lymphocytes (TILs) - T cells that are naturally found in the patients tumor are used that best recognize the patients tumor cells. These are grown in the laboratory and treated with cytokines which are infused back into the patient which signals the immune system to attack the tumor cells
- CAR T-cell therapy - patients T-cells are extracted and genetically engineered to bind to specific antigens in the cancer cell and destroy the cancer cells
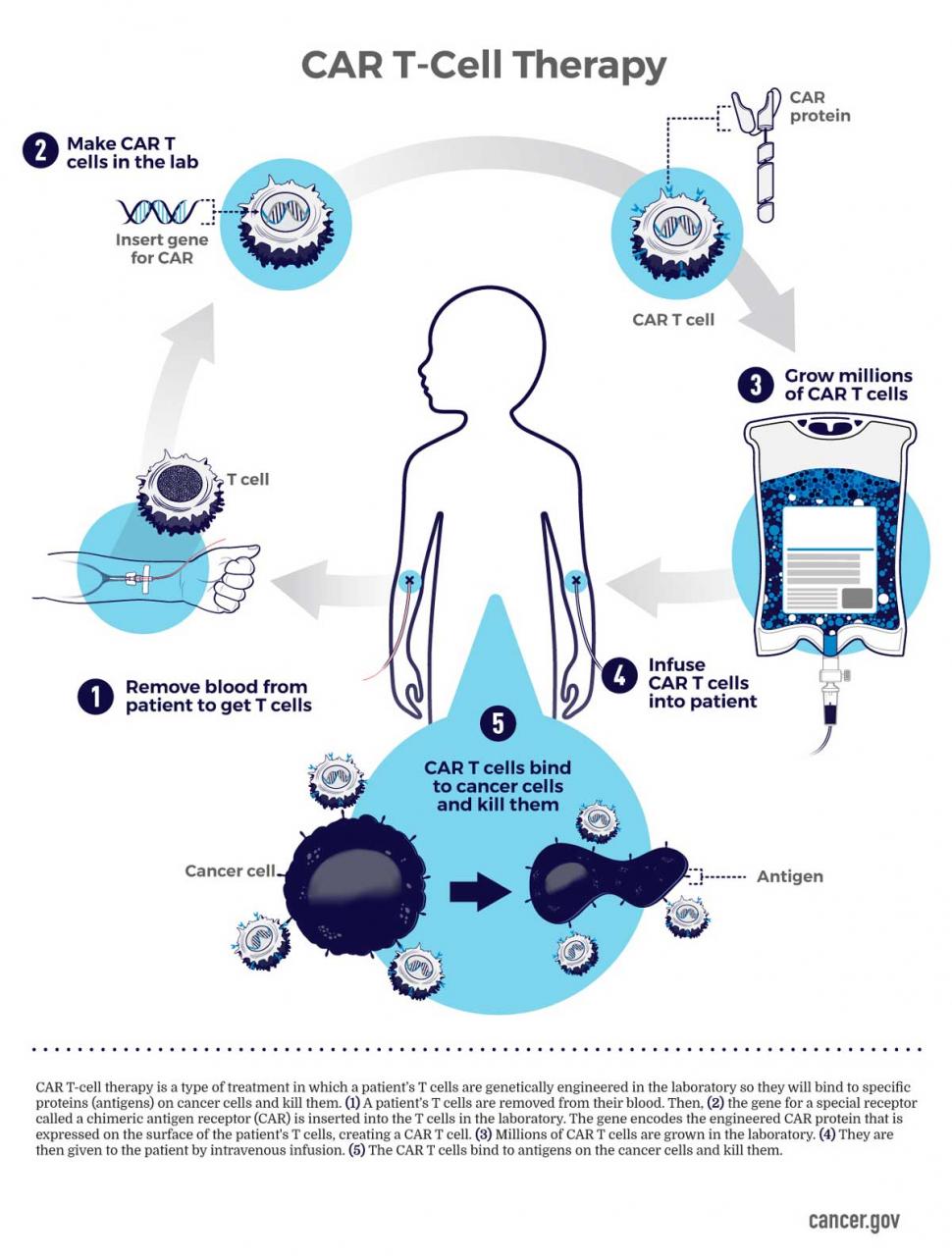
CAR T-Cell Therapy. Source: National Cancer Institute (NCI).
Updated: December 21, 2023
Suggested Citation
SEER Training Modules: Stem Cell Transplants. U.S. National Institutes of Health, National Cancer Institute. Cited 27 February 2026. Available from: https://training.seer.cancer.gov.




