Neoplasm Information OR Histology Search Results Webpage
On this page...
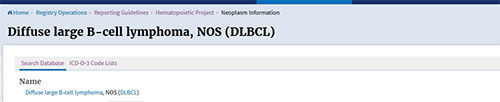
Learning how to navigate the database is vital if you are going to successfully abstract Hematopoietic neoplasms. This next section will go through each of the sections of a histology search results webpage, using 9680/3: Diffuse Large B-cell lymphoma (DLBCL) as a search example.
Sections of a Histology Search Results Page
Name: Under the Search Database and ICD-O-3 code lists is the name field. This is the preferred terminology for the searched histology per the current edition of the WHO Blue Book for Hematolymphoid tumors. This name may change from one edition to another. The preferred terminology in the Hematopoietic Database is based on the 5th edition of the WHO Blue Book for Hematolymphoid Neoplasms.
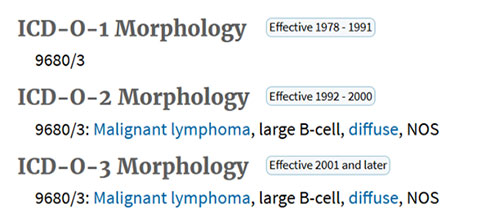
Histology (history): This is the ICD-O-3 term for the neoplasm (current edition is ICD-O-3.2, which was implemented in 2021). The ICD-O-3 term may be the same or different from the name, which is based on the current WHO edition (5th edition released November 2024).
Reportability:Reportability is based on when the neoplasm first became reportable. This may be different from when the ICD-O code was implemented.
For example, 9715/3: Anaplastic large cell lymphoma, ALK-negative was implemented in 2021 (ICD-O-3.2 update). The histology code 9715/3 can only be used for 2021; however, the actual term is reportable for 1978 forward since it’s a lymphoma.
- Per the Heme DB, registrars are instructed to code 9702/3 for cases diagnosed prior to 2021.
Within the Hematopoietic database (but no longer available publicly) are the ICD-O-1 and ICD-O-2 fields that are used to determine reportability. These two fields were recently removed since registrars found them confusing, and they were not needed for abstracting.
See “The Hematopoietic Manual: Reportability” for more information
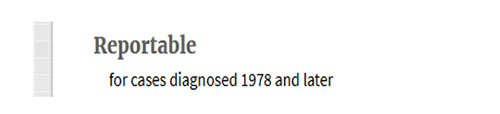
Note: Reportability for neoplasms in the Hematopoietic Database does not include information from MOTNAC. Reportability starts with ICD-O-1, implemented in 1978
Primary Site: This next section provides guidance determining the primary site. For this histology, you you’ll be referred to Modules 6 and 7 to determine primary site. DLBCL can occur almost anywhere in the body.
- For some histologies, such as Leukemias, the default primary site (C421) is listed here.
Diagnosis Year: This section is very important. The information provided for a given histology may vary depending on the WHO edition (blue book) used as the database reference. Any changes in the fields below this box are year-specific. By selecting the appropriate year, you ensure that you are viewing the correct information. This is especially critical for terms that have been reclassified over time. Accuracy will become even more important when the U.S. adopts ICD-O-4, as many terms will be assigned their own unique ICD-O-4 codes.
Note: When you open the database, it defaults to the current year and will remain on that year until you change it. If you select a different year, the database will stay on that year until you change it again or close the database.

Abstractor notes: Right above the abstractor notes is where you’ll find a link to the current Hematopoietic manual. This is available in every histology.
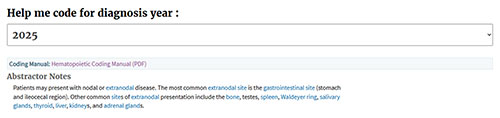
Abstractor notes are very important. They provide additional information on primary site, stage, unique characteristics of the histology, or other things to look for. For some histologies, there are various stages (chronic, blast, etc.) that are still considered the same primary, and if that is the case, then the information is provided in the abstractor notes.
Diagnostic Confirmation: This data item documents the method used to confirm the cancer diagnosis (e.g., microscopic examination, genetic testing, imaging).
Depending on the presentation of the patient and the suspected neoplasm, a peripheral blood smear may be done first. If a diagnosis is made based on the peripheral blood smear, that is a diagnostic confirmation 1 for positive histology. Flow cytometry is commonly done with peripheral blood smears. Genetic testing may also be done. If either flow cytometry or genetic testing is done and is positive, and the physician updates the histology based on the positive immunophenotyping or genetics then diagnostic confirmation would be 3.
If a patient has a suspected blood neoplasm (myelodysplastic syndrome, myeloproliferative neoplasm, or leukemias), a bone marrow biopsy is commonly done. If a diagnosis is made from a bone marrow biopsy only, then that would be a diagnostic confirmation of 1. Immunophenotyping and genetics are commonly done with a bone marrow biopsy.
Some histologies will always require a Diagnostic Confirmation of 3 because the diagnosis is defined by genetic markers. For example, 9871/3: Acute Myeloid Leukemia with inv(16)(p13.1q22) or t(16;16)(p13.1;q22), CBFB/MYH11 cannot be diagnosed based solely on a peripheral blood smear or bone marrow biopsy—genetic testing is necessary. Many hematopoietic neoplasms, particularly acute myeloid leukemias and acute lymphoblastic leukemias, are defined by their genetic features. This approach is also increasingly applied to lymphomas, such as cyclin D–positive mantle cell lymphoma.
Diagnostic Confirmation code 2 is rarely used and applies only to fine-needle aspirates (FNAs). It is typically seen with lymphomas, not blood-based cancers. Often, an FNA is performed on a lymph node, followed by flow cytometry, which either confirms the diagnosis or identifies a more specific subtype. In these cases, the Diagnostic Confirmation would be coded as 1 or 3 rather than 2. Because determining the precise histology is crucial for hematopoietic neoplasms, it is uncommon for an FNA to be the sole diagnostic test.
See “The Hematopoietic Manual: Diagnostic Confirmation” section for more information
Module Rule: Some histologies may be associated with a specific module rule. This does not mean that the module rule is the rule that is applicable for the case though. Registrars still need to go through the rules to determine which rule is applicable.
- For DLBCL, Module 6, PH11 and PH13 are rules that pertain to DLBCL. PH11 and PH13 will not apply to all DLBCLs.
Alternate Names
This section lists all the alternate terms that a histology code can have. Over the years through the different WHO editions, names continue to evolve and change. Names used in the 70s and 80s are very different than the names used today. Some of the terms come from old ICD-O-1, 2 or 3 codes that are no longer valid, but may still be used by some pathologists.
The alternate names are based primarily on the current WHO edition for Hematolymphoid Tumors. Some histologies have subtypes, which are listed as alternate names. Additional alternate names come from ICD-O-3.
Definition
This is the definition from the current WHO edition for Hematolymphoid tumors.
Definitive Diagnosis
This field identifies the method used to establish a diagnosis. Most hematopoietic diseases require a histologic diagnosis, usually from a biopsy (including bone marrow). For Hematopoietic neoplasms defined by genetic features, diagnosis is only possible through genetic testing. A small number of hematopoietic neoplasms can be diagnosed clinically, but these are usually broad, nonspecific terms such as lymphoma, NOS or leukemia, NOS.
Genetics and Immunophenotyping
This field lists the most common genetic findings and immunophenotyping results associated with each neoplasm (when applicable). It is not a complete list, since new discoveries and updates occur frequently in clinical practice. If a pathologist or treating physician revises a histology based on genetic or immunophenotyping results that are not included in the Hematopoietic Database, you may still use that information to assign diagnostic confirmation.
Treatments
This section lists the generic categories of applicable treatment options for the searched histology. These can include chemotherapy, radiation, immunotherapy, and/or hormone therapy. Registrars are encouraged to use SEER*RX, the NCCN guidelines, or the NCI PDQ for specific treatment information.
“”Transformations to”” and “”Transformations from””
The idea of transformation is unique to hematopoietic neoplasms. Some neoplasms are indolent (slow growing, chronic), while others are aggressive (fast growing, acute). Indolent neoplasms can sometimes “transform” into more aggressive forms.
- The “Transformations to” field (when present) are aggressive or acute neoplasms that the chronic or indolent neoplasm transform to. If a chronic/indolent neoplasm can transform to an acute/aggressive neoplasm, the Heme DB will show the acute neoplasm in the “Transformations to” section.
- The “Transformations from” field (when present) are indolent or chronic neoplasms that have transformed to the aggressive or acute neoplasm. Acute neoplasms may have multiple histologies listed in the “Transformations from” field. Histologies listed in the “Transformations from” field are chronic.
To use the chronic/acute rules, the “Transformation to” and “Transformation” from fields must agree with one another.
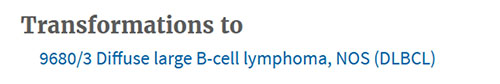
This screen shot of the database shows that the histology (which is 9823/3-CLL/SLL) transforms to 9680/3, DLBCL (the acute neoplasm). The DLBCL may be a second primary depending on when it was diagnosed in relation to the CLL/SLL. Multiple primary rules M8-M13 are written for neoplasms that transform.
This screen shot is from 9680/3 (DLBCL) and shows that many lymphomas transform to DLBCL, including the CLL/SLL at the bottom.
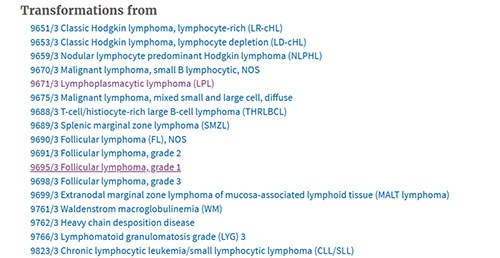
Only the most common transformations are shown in the Hematopoietic Database. It is possible to have other transformations.
If the “transformation to” and “transformation from” fields are blank, that means there are no known transformations and Rules M8-M13 do not apply. Even if the physician states that something has transformed, do not use Rules M8-M13 if there are not neoplasms listed.
Same Primaries
Same primaries occur when two diagnoses represent the same disease. For example, a specific non-Hodgkin lymphoma (9690/3: Follicular Lymphoma) and a non-Hodgkin lymphoma, NOS (9591/3, NHL, NOS) are considered the same primary. These designations are applied in the multiple primaries calculator. Only use the multiple primaries calculator when you are instructed to do so (See Rules M7 and M15).
Remaining Fields
These are the fields in the database that are helpful to registrars as they are coding their cases. Other fields include the applicable ICD-10 (Cause of Death) codes and ICD-10-CM (Clinical) codes, common signs and symptoms, and common diagnostic tests done during the clinical workup, progression and transformation, and related epidemiology and mortality data.
At the end of the database, you’ll find the source files used to compile the information. The main references include:
- The current edition of the WHO Classification of Hematolymphoid Tumors (Blue Book)
- ICD-O-3.2 for histology codes
- The National Cancer Institute’s Physician Data Query (PDQ)
As of Summer 2025, the Hematopoietic Database is based on the WHO 5th edition Blue Book for Hematolymphoid Tumors.
Updated: December 2, 2025
